
Clostridia Bacteria & the Link to ASD Behavior & Neurodevelopmental Problems
By Kurt N. Woeller, D.O.
Clostridia are a group of pathogenic and non-pathogenic bacteria that can normally inhabit the digestive system of humans. Certain strains of clostridia can be very problematic leading to serious illness and death. Well recognized clostridia bacteria are the strains that cause tetanus, botulism and inflammatory bowel disease. Inflammatory bowel, for example, can be triggered by Clostridium difficile (C. diff.) in a condition called pseudomembranous colitis. It’s estimated that upwards of 29,000 people in the United States die yearly from a C. difficile related problems (1). However, there are other strains of clostridia that can be problematic too and other chemicals produced by these bacteria that have toxic effects beyond those that trigger the intestinal problems often associated with C. difficile.
In 2010, William Shaw, Ph.D. from Great Plains Laboratory in Lenexa, KS published a paper in Nutritional Neuroscience titled “Increased urinary excretion of 3-(3-hydroxy-phenyl)-3-hydroxypropionic acid (HPHPA), an abnormal phenylalanine metabolite of Clostridia spp. in the gastrointestinal tract, in urine samples from patients with autism and schizophrenia.” (2). This important paper discusses the fact that a toxic compound called HPHPA was found in very high concentrations in urine samples of children with autism compared to age and sex appropriate controls, and in adults with recurrent diarrhea due to Clostridium difficile infections. In fact, the highest value was 7500 mmol/ml creatinine, a value 300 times the median normal value for an adult, was found in a an individual with acute schizophrenia. In this particular patient with schizophrenia their psychosis remitted after a treatment course with oral vancomycin.
For years, through my private consultations and educational programs, I have been recommending that parents and caregivers of individuals with autism perform Organic Acid Testing (OAT) from Dr. Shaw’s Great Plains Laboratory for the evaluation of HPHPA and other metabolic markers known to negatively influence body and brain chemistry. The role of clostridia infections in neurological health had been poorly understood until Dr. Shaw’s paper in 2010, but the clinical experience of many integrative medicine doctors working with special needs individuals who recognized digestive pathogens and their role in negative health outcomes dates back many years. The major impact I see clinically in patients with elevated HPHPA (as well as another clostridia bacteria toxin called 4-Cresol), particularly in individuals on the autism-spectrum, is erratic, aggressive and self-injurious behavior. Sometimes these behaviors are so severe the person is heavily medicated in attempts to control the problems.
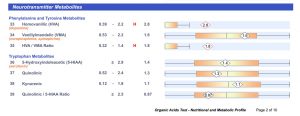
The two images listed below represent high HPHPA and 4-Cresol, respectively, as is commonly seen through the Organic Acids Test (OAT) from Great Plains Laboratory.
 This image is from the Clostridia Bacteria Markers section of the OAT. The elevation of HPHPA is quite high. Notice that one of the strains of clostridia known to produce this toxin is Clostridia botulinum, the bacteria known to cause botulism.
This image is from the Clostridia Bacteria Markers section of the OAT. The elevation of HPHPA is quite high. Notice that one of the strains of clostridia known to produce this toxin is Clostridia botulinum, the bacteria known to cause botulism.
 Common toxin produced by clostridia is 4-Cresol. In fact, 4-Cresol is specific to certain strains of Clostridia difficile. It too, like HPHPA, is extremely toxic.
Common toxin produced by clostridia is 4-Cresol. In fact, 4-Cresol is specific to certain strains of Clostridia difficile. It too, like HPHPA, is extremely toxic.
Biochemically 4-Cresol (and HPHPA) specifically interfere with a converting dopamine enzyme called Dopamine Beta-Hydroxylase (3). This enzyme is responsible for converting dopamine into the neurotransmitter norepinephrine. Norepinephrine is the neurochemical most responsible for vigilant concentration, whereas one of the roles dopamine is in alertness (4). One of the major problems recognized with the accumulation of dopamine and the negative effects it has on brain function has to do with neurodegeneration associated with oxidative stress.
A research article in 2008 titled “Unregulated cystolic dopamine causes neurodegeneration associated with oxidative stress in mice” (5) discusses the biochemical consequences of excess dopamine:
• Dopamine is a reactive molecule compared with other neurotransmitters and dopamine degradation naturally produces oxidative species.
• More than 90% of dopamine in dopamine neurons is stored in abundant terminal vesicles and is protected from degradation.
• A small fraction of dopamine is cytosolic and it is the major source of dopamine metabolism and presumed toxicity.
• Cytosolic dopamine undergoes degradation to form a compound called 3,4-dihydroxyphenylacetic acid (DOPAC) and Homovanillic Acid (HVA) as well as hydrogen peroxide via the monoamine oxidase pathway. The HVA is a marker measured on the Organic Acids Test (see image 3 below).
• Dopamine also undergoes oxidation to form superoxide, hydrogen peroxide and o-quinone and reacts with cysteine residues on glutathione, thus rendering glutathione ineffective.
• Dopamine oxidation can also form cysteinyl-dopamine and cysteinyl-DOPAC conjugates which are neurotoxic.
• These biochemical abnormalities caused by excess dopamine may cause severe neurodegeneration of neural pathways that utilize dopamine as a neurotransmitter.
The elevated HVA is often seen with high HPHPA and/or 4-Cresol. The Dopamine-Beta-Hydroxylase enzyme is inhibited causing excess dopamine and the byproduct HVA.
Prior to this research article, a paper in 2000 titled “Short-term benefit from oral vancomycin treatment of regressive-onset autism” (6) discussed the benefit to a group of autistic children:
• 11 children with regressive-onset autism were recruited for an intervention trial using a minimally absorbed oral antibiotic.
• Entry criteria included antecedent broad-spectrum antimicrobial exposure followed by chronic persistent diarrhea, deterioration of previously acquired skills, and then autistic features. Short-term improvement was noted using multiple pre and post-therapy evaluations. These included coded, paired videotapes scored by a clinical psychologist
blinded to treatment status.
• These noted improvements in 8 of 10 children studied. Unfortunately, these gains had largely waned at follow-up.
The authors involved in this research summarized with the following statement, “although the protocol used is not suggested as useful therapy, these results indicate that a possible gut flora-brain connection warrants further investigation, as it might lead to greater pathophysiologic insight and meaningful prevention or treatment in a subset of children with autism.”
Treatment of clostridia bacteria may require antibiotics, but there are effective botanical protocols that have shown successful in eradicating these bacteria too. These botanicals are often used in conjunction with other nutritional supplements to support digestive health and cellular metabolism. It’s important for both the parent and practitioner taking care of an individual with autism that the role of clostridia bacteria and their related toxins is just one piece of a complex puzzle of various underlying comorbid conditions often seen in this population of individuals. Therefore, the random use of supplements such as certain amino acids like tyrosine and/or phenylalanine may worsen the behaviors seen in autism because certain clostridia bacteria use these amino acids to make their respective HPHPA and 4-Cresol toxins. In my practice the Organic Acids Test from Great Plains Laboratory is the first step in medical testing for any individual on the spectrum.
Dr. Kurt N. Woeller is the medical director of Sunrise Complementary Medical Center in Bend, Oregon (USA). In addition to being a practicing clinician, he is an author of several books on autism, educator and international speaker on the topic of integrative medicine for autism. He runs educational programs for health practitioners through his online academy at www.IntegrativeMedicineAcademy.com and for parents and caregivers through his website called Autism Recovery System – www.AutismRecoverySystem.com.
References:
(1) Leesa FC, Mu Y, Bamberg WM, et al. “Burden of Clostridium difficile infection in the United States.” N Engl J Med. 2015;372:825-834.
(2) Shaw, W. “Increased urinary excretion of a 3-(3-hydroxyphenyl)-3-hydroxypropionic acid (HPHPA), an abnormal phenylalanine metabolite of Clostridia spp. in the gastrointestinal tract, in urine samples from patients with autism and schizophrenia.” Nutr Neurosci. 2010. 13(3):135-43.
(3) Goodhart, PJ, et. al. “Mechanism-based inactivation of dopamine beta-hydroxylase by p-cresol and related alkylphenols.” Biochemistry. 1983 Jun 21; 22(13):3091-6
(4) John D. Hunt. Associate Clinical Professor of Psychiatry, Vanderbilt University Medical School, Nashville, Tennessee; CEO & Medical Director, Center for Attention and Brain Function, Nashville, Tennessee “Functional Roles of Norepinephrine and Dopamine in ADHD: Dopamine in ADHD”Associate Clinical Professor of Psychiatry, Vanderbilt University Medical School, Nashville, Tennessee; CEO & Medical Director, Center for Attention and Brain Function, Nashville, Tennessee.
(5) Linan Chen, et al. “Unregulated cytosolic dopamine causes neurodegeneration associated with oxidative stress in mice.” J. Neurosci. 2008 28, 425–433
(6) Sandler RH et.al. “Short-term benefit from oral vancomycin treatment of regressive-onset autism” J Child Neurol. 2000. 15(7):429-35




